Do you suffer from dry, itchy eyes? If so, then an allergic reaction could be the culprit. Allergies can cause eye-related symptoms, including redness, itching, and dry eyes.

If your eyes feel less than their best, you may be one of the millions wondering, ‘Can allergies cause dry eyes?” The answer is yes, and I have various treatment options listed below.
Take note: This post contains a lot of information and answers to your dry eye questions. For convenience, I’ve added this table of contents so you can quickly click a link to find your topic. You can also read the entire post if you prefer.
Need some help finding time to take better care of yourself? Get your FREE copy of the Self-care Starter Guide HERE!

You’re probably familiar with the nasal symptoms if you already suffer from allergies.
Inflammation in your sinuses and airways produces uncomfortable symptoms and can be mild to severe. Nasal symptoms of allergies can include:
- Sneezing
- Itching of the nose or roof of the mouth
- Runny nose
- Nasal congestion (stuffy nose)
- Sore throat
Other symptoms of allergies can include (click on the links to learn how to relieve these less common symptoms):
- Dry mouth
- High blood pressure
- Allergies can even cause snoring and lead to obstructive sleep apnea, a type of gasping-for-breath breathing while asleep
- Hearing loss
Unfortunately, allergy season can cause severe discomfort to allergy sufferers’ eyes.
Thankfully, there are at least 14 self-care tips and home remedies to relieve your dry eye symptoms.
I’ve been a nurse for over 32 years, so I’ve only included the tips that healthcare providers in this specialty area recommend or have been proven effective through scientific research.
Why are My Eyes So Dry? Can Allergies Cause Dry Eyes?
When someone has allergies, it means they’ve had an allergic reaction to a foreign object (an allergen), which causes an immune response. An allergy develops after the immune system overreacts to something that doesn’t affect others.
When the allergen comes in contact with specific mast cells, those cells respond by releasing chemicals and substances to counter the allergen.
A well-known chemical is called histamine, and its job is to help the body fight the allergy. Histamine causes tiny blood vessels in the eye to leak, making the eyes itchy. Red and watery eyes are also very common.
Many people don’t realize that seasonal allergies can be the underlying cause for their dry eyes but understanding why this happens is essential to find relief from the eye discomfort.
In particular, avoiding common eye allergy triggers can help your eyes feel better.

Common Eye Allergy Triggers
The common allergy triggers can include:
Outdoor allergens include pollen from:
- Grass
- Trees
- Weeds
Indoor allergens like
- Pet dander
- Dust mites
- Mold
Environmental irritants like:
- Smoke from cigarettes or cigars
- Exhaust fumes
- Perfume
Additionally, knowing the common symptoms of dry eyes, self-care, and treatment for eye allergies can help determine if your dry eyes may require further evaluation from a healthcare provider. Some eye allergies have similar symptoms to some diseases of the eye.
Eye symptoms from allergies should resolve within one to two weeks after the allergens are no longer in the air.
Dry Eye Symptoms From Seasonal Allergies
Red and irritated eyes can be symptoms of eye allergies.
Although these eye symptoms typically accompany the nasal and other symptoms, they can occur independently from other typical allergy symptoms and the nomenclature moves away from seasonal allergy symptoms and centers on ocular allergies, also known as allergic conjunctivitis.
Other eye allergy symptoms include:
- Itching
- Burning
- Redness
- Clear, watery discharge

Ocular Allergies
Five types of ocular allergies produce dry eye symptoms:
- Seasonal (or perennial) allergic conjunctivitis
- Vernal keratoconjunctivitis
- Atopic keratoconjunctivitis
- Contact allergic conjunctivitis
- Giant papillary conjunctivitis
These eye conditions are listed below, along with a description of their unique symptoms and severity.
Seasonal Allergic Conjunctivitis
The most commonly seen eye allergy is seasonal allergic conjunctivitis (SAC), which, depending on the type of allergy, can cause symptoms in spring, summer, and fall. SAC is the condition most often confused with dry eye syndrome.
In addition to the typical eye allergy symptoms of
- Red eyes
- Itching
- A burning sensation
- Clear discharge
Conjunctivitis is the term used to describe inflammation of the conjunctiva, which is the mucous membrane that lines the exposed portion of the eyeball and inner surface of the eyelids. The inflammation is caused by the frequent rubbing of itchy eyes, which makes the symptoms worse and can cause an infection of the surface of the eye.
People with SAC may also have dark circles under their eyes. These dark circles, called allergic shiners, may become chronic.
Other symptoms of SAC include the usual symptoms of hay fever and allergic rhinitis, such as a runny nose, sneezing, and nasal congestion.
Another version, perennial allergic conjunctivitis (PAC), occurs year-round. Its symptoms are the same but typically milder. Indoor allergens cause it.
Vernal Keratoconjunctivitis
Vernal keratoconjunctivitis is a more serious eye allergy compared to SAC or PAC. It can occur year-round, but the symptoms can become heightened during the usual allergy seasons.
Vernal keratoconjunctivitis can impair vision if left untreated.
The symptoms include:
- Itching
- Excessive tearing
- Thick mucus production
- Photophobia (sensitivity to light)
This eye allergy occurs most commonly in boys and young men, and most patients have a co-existing diagnosis of eczema or asthma.
Atopic Keratoconjunctivitis
Atopic keratoconjunctivitis is also more serious than SAC or PAC and, if left untreated, can scar the cornea and its fragile membrane.
Symptoms are similar to vernal keratoconjunctivitis and can also occur at any time of the year. The symptoms are:
- Severe itching of the eye
- Burning
- Redness
- Excessive thick mucus production, especially during sleep, may cause the eyelids to stick together.
This eye allergy affects mostly older males who also historically have had allergic dermatitis.
Contact Allergic Conjunctivitis
Contact allergic conjunctivitis may be caused by irritation to the eye’s surface from either contact lenses or by proteins from tears that bind to the surface of the contact lens.
In addition to the usual eye redness and itching, symptoms include mucous discharge and discomfort while wearing contact lenses.
Giant Papillary Conjunctivitis
Giant papillary conjunctivitis is also a condition specific to contact lens wearers in which contact allergic conjunctivitis has become more severe and papules, or individual fluid sacs, have formed in the upper lining of the inner eyelid.
Symptoms include:
- Itching
- Puffiness
- Tearing
- Mucous discharge
- Blurry vision
- Discomfort while wearing contact lenses
- Foreign body sensation (feels like something is in the eye)
How to Treat Dry Allergy Eyes With Self-care and Lifestyle Changes
Hopefully, I’ve shown you the answer to your question: can allergies cause dry eyes? It’s a definite yes.
The good news is that self-care and lifestyle changes can be implemented to improve dry eyes caused by allergies.
Changing your self-care, routine, and home to avoid allergy triggers is an effective first step toward managing or preventing dry eyes due to seasonal allergies. In my experience, self-care, especially for prevention, can be powerful!
My referral and affiliate links are below. If you click through & make a purchase, I may receive a commission at no additional cost to you. My full disclosure can be viewed for details.
Looking for a way to stay motivated to take better care of yourself? Click my affiliate link to check out my Bible study.

Self-care and Lifestyle Changes
- Avoid going outdoors when pollen counts are high – during allergy seasons, particularly at dawn or dusk.
- Wear wrap-around glasses or sunglasses outdoors or doing yard work to keep pollen and wind out of your eyes.
- Use smoking cessation strategies and avoid secondhand smoke.
- Wash your hands after petting any cat or dog. Wash your clothes when you visit friends with pets.
- Monitor the side effects of the medications you take, like antacids, beta-blockers, antidepressants, and anxiety medications, because many can cause dry eye symptoms.
- Wear glasses instead of contacts.
- Minimize hair dryer usage.
- Talk to your healthcare provider about adding omega-3 fatty acids (found in salmon, sardines, herring, tuna, menhaden, walnuts, olive oil, and cod liver) to your diet for dry eye relief. <source>
- Apply cold compresses to your eyes.
- Avoid sitting in front of a fan.
- Take frequent breaks from looking at digital screens, reading, or crafts (sometimes we blink less when focused).
- Avoid being around smoke from fireplaces, bonfires, or other smoke sources.
- Wear goggles when working in a woodshop, doing yard work with debris, or even dusting your home.
- Seek routine eye care by having annual eye exams.
Over-the-Counter (OTC) Medications to Treat Allergy Eyes
Nonprescription (over-the-counter) eye drops and oral medications are frequently used for the short-term relief of some symptoms.
Because many over-the-counter eye drops (and oral antihistamines do as well) contain antihistamines that reduce tear production, eye specialists recommend using OTC preservative-free artificial tears, along with allergy drops, to keep your eye’s surface from drying out.
Don’t use any eye drops or medications for longer than a week without a healthcare provider’s guidance. OTC eye drops may have side effects that make things worse, and an eye doctor may be able to offer you prescription drops that are more effective with fewer side effects.
Effective changes in your home may include:
- Close windows and use your air conditioner in your car and home, especially during the high pollen season (spring, summer, and fall).
- Add air purifying devices to the rooms where you spend most of your time to reduce indoor allergens.
- Using mattress and pillow covers that are dust-mite-proof.
- Using a dehumidifier to control mold growth.
- Avoid using fans in windows, bringing pollen and mold into your home.
- Regularly cleaning your home to remove the pet dander and dust that collects on surfaces.
Unfortunately, many of the allergens that trigger eye allergies are in the air, so you’re not always able to avoid them as simply as you’d like.
In some cases, prevention is the most effective solution to improve your quality of life. So, consider seeing an allergist for allergy testing, allergy shots, and a preventative treatment plan.

When to See the Eye Doctor for Dry Eyes
When should you make an appointment to see an eye doctor for your dry eye symptoms?
- If you believe you may have one of the five specific dry eye conditions listed
- Your eye irritation doesn’t resolve with self-care within 1-2 weeks
- If your condition lasts after the pollen counts have decreased
The best way to identify the root cause of your dry eyes is to get a comprehensive eye exam from an optometrist or ophthalmologist. If you have any concerns, don’t wait. Schedule an appointment because different eye conditions have different treatments.
An eye specialist will ask about your symptom history and perform an eye examination which may include an external examination of the eye, including:
- Lid structure and blink dynamics
- Eyelids and cornea using bright light and magnification
- Measurement of the quantity and quality of tears. Special dyes may be used to observe tear flow and emphasize changes to the eye’s outer surface caused by insufficient tears. <source>
Typical Treatment Recommend by Eye Specialists
Mast cell stabilizers or antihistamines to stop the histamine production from the mast cells are typically recommended to treat allergy symptoms. Still, antihistamine eye drops may also be recommended if the symptoms are affecting your eye, especially when you have ocular allergies. Avoiding allergens and using artificial lubricants are also standard treatments.
Recommended treatment regimens may include:
- Prescription eye drops or ointments
- Over-the-counter articifical tears to add tears or to improve tear secretion
- Warm compresses on the affected eye
- Massaging your eyelids (only do this if it is recommended)
- Certain eyelid cleansers
- Blocking your tear ducts by placing silicone or gel plugs (called punctal plugs) in your tear ducts to help your natural tears stay in your eyes longer (these plugs may stay or be removed later)
- Lid procedures, depending on the condition
Unfortunately, eye allergies can lead to dry eye, and having dry eye can lead to eye allergies.
There is another condition with similar symptoms called dry eye syndrome, but treatment is different for eye allergies and dry eye.
Dry eye treatment typically addresses the underlying inflammation and the meibomian glands.
What is Dry Eye Syndrome?
Dry eye is common, with over 16 million people in the United States diagnosed with it. Because so many have this condition, your eye specialist can offer several dry eye treatment options.
Also known as dry eye disease, the American Academy of Opthmalogy defines dry eye as a condition where you do not produce enough tears, or your tear production is inadequate and only produces poor-quality tears. The causes of dry eye may include:
- Meibomian gland dysfunction (MGD) – the meibomian glands in your upper and lower eyes produce an oil essential to forming healthy tears, providing the lipid layer of the tear film. This layer of oil keeps the surface of your eye moist by reducing tear evaporation.
- Age and gender – >50 years old, tear production decreases with aging
- Medications -antihistamines and decongestants decrease tear production. Sometimes, treating an eye allergy with these medications can lead to dry eye syndrome
- Environmental factors – allergens, low humidity, smoke, and chemicals
- Not enough blinking – digital eye strain (while reading on a screen like a phone or a computer)
- Allergies
- Hormonal problems
- Diabetes
- Autoimmune disorders like rheumatoid arthritis, lupus, Sjogren’s syndrome, & thyroid disease
- Blepharitis
- Refractive eye surgery
- Long-term contact lens wear
This condition is multifactorial, with an inflammatory component that can markedly worsen the impact on the ocular surface. Meibomian gland dysfunction contributes to the inflammatory process. <source>
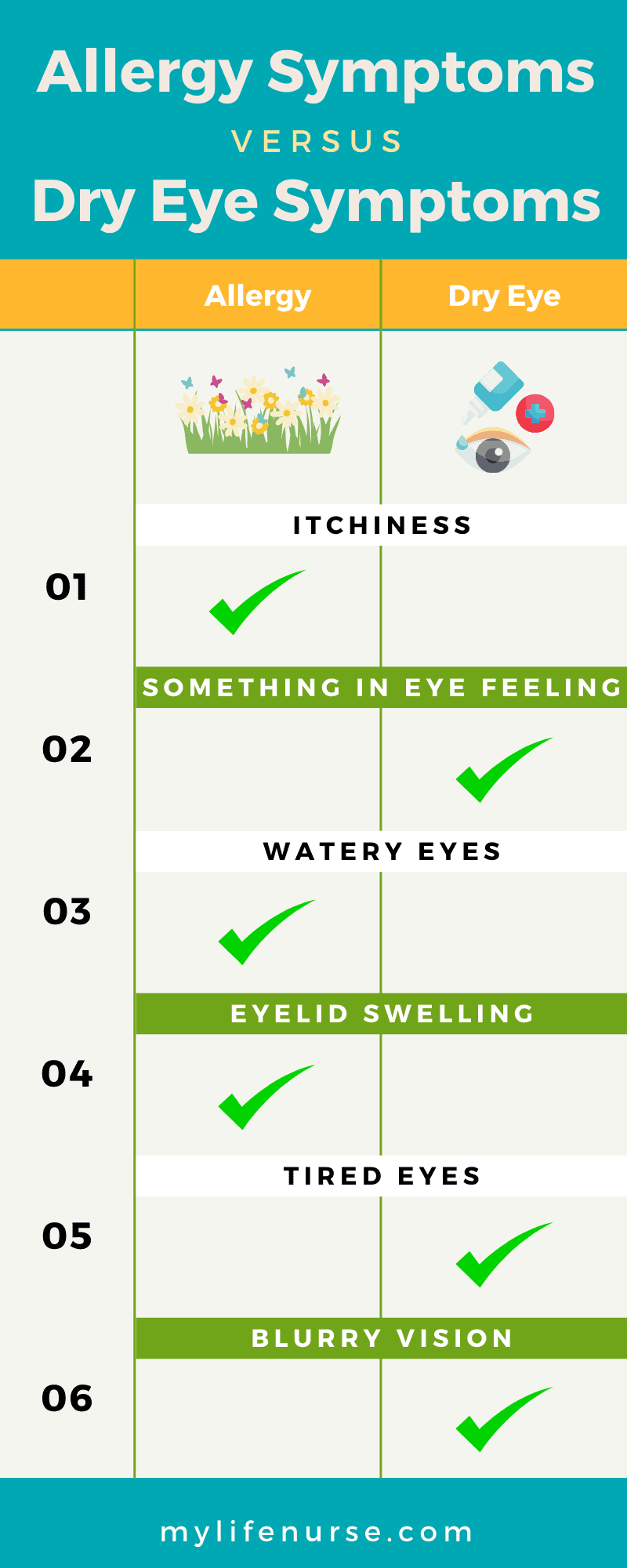
Differentiating Allergy and Dry Eye Symptoms
The main difference in symptoms between allergic conjunctivitis and dry eye is intense itching.
Itching may occur with dry eye syndrome, but it is typically more intense with allergic conjunctivitis. Itching associated with a runny nose or watery eyes may be a sign it’s more likely related to allergies.
The most common symptoms of dry eye syndrome include:
- Scratchy sensation
- Foreign body sensation (feels like something is in your eye)
- Stinging
- Burning
- Redness
- Watery eyes
- Sensitivity to light
- Mild itch
- Blurry vision
- String mucus discharge
In closing, while there are certainly times when self-care, oral medications, and home remedies can effectively stabilize dry eye symptoms, there are also times when it can be difficult to determine if allergies are the only reason for your eye discomfort.
If you find your dry eye symptoms are starting to become a chronic condition, you believe you may have symptoms of any of the ocular allergy conditions listed in this article, or you’re struggling to tell the difference between dry eye and allergies, I encourage you to schedule an appointment with an eye specialist as soon as possible.
Getting an ocular tissue examination is the best (and relatively inexpensive) path to an appropriate treatment plan so you find relief.
You do not have to live with chronic dry eyes.
Exhausted & Overwhelmed?
This Self-care Starter Guide will show you 3 simple steps to take RIGHT NOW to take better care of yourself.
Be sure to grab yours!
Get your FREE copy of the Self-care Starter Guide HERE!
Thanks for reading! Know someone who would benefit from reading this post? Share it on social media!

Ready for more? Here are my latest posts!
- 9 Must-Read Blog Posts to Manage High Blood Pressure Naturally
- Overcome Self-care Barriers with 4 Easy Tips
- 4 Easy Ways to Get Your Spouse to Eat Healthy Food
- 5 Easy Ways to Find Me-Time in Your Busy Schedule
- How to Try New Vegetables When You Hate to Eat Veggies
This post was originally published on July 13, 2023.

Be sure to grab your FREE Self-care Starter Guide! Lisa Kimrey is a 33-year veteran registered nurse (RN), speaker, and author of the Bible study, The Self-care Impact: Motivation and Inspiration for Wellness. At Mylifenurse, Lisa combines her nursing expertise with Scripture-based encouragement to show readers who serve and care for others how to begin and maintain their self-care journey – without feeling guilty or overwhelmed – to feel happy, healthy, and rejuvenated.